Diagnosing XLH
Learn more about how to accurately diagnose XLH through testing.
Your patients may likely experience ongoing XLH-related symptoms and may not mention all of them or may even downplay them.
Most adults with XLH have been living with symptoms since childhood and may develop new complications later in life. Over time, they may get used to the chronic pain, fatigue, and muscle dysfunction.2,3,5 As a chronic and progressive disease, XLH requires careful monitoring and early management of symptoms.










Because some symptoms of XLH may not be visible like chronic pain or fatigue, it is important to listen to your patients. Getting an accurate diagnosis can help you manage the full range of symptoms they may be experiencing.

Learn more about how to accurately diagnose XLH through testing.

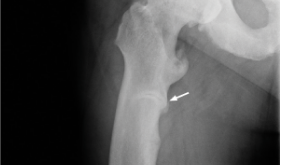
Manage XLH early to prevent progressive bone damage.
Watch videos to get more information about how XLH affects the body.
Set up time with a representative to talk more about XLH, or sign up for news and information about XLH.
References:
1. Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL. A clinician's guide to X-linked hypophosphatemia. J Bone Miner Res. 2011;26(7):1381-1388. doi:10.1002/jbmr.340 2. Linglart A, Biosse-Duplan M, Briot K, et al. Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr Connect. 2014;3(1):R13-R30. doi:10.1530/EC-13-0103 3. Skrinar A, Dvorak-Ewell M, Evins A, et al. The lifelong impact of X-linked hypophosphatemia: results from a burden of disease survey. J Endocr Soc. 2019;3(7):1321-1334. doi:10.1210/js.2018-00365 4. Hamilton AA, Faitos S, Jones G, Kinsley A, Gupta RN, Lewiecki EM. Whole body, whole life, whole family: patients' perspectives on X-linked hypophosphatemia. J Endocr Soc. 2022;6(8):bvac086. doi:10.1210/jendso/bvac086 5. Giannini S, Bianchi ML, Rendina D, et al. Burden of disease and clinical targets in adult patients with X-linked hypophosphatemia. A comprehensive review. Osteoporos Int. 2021;32(10):1937-1949. doi:10.1007/s00198-021-05997-1 6. Ruppe MD. X-linked hypophosphatemia. In: Adam MP, Everman DB, Mirzaa GM, et al., eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; February 9, 2012. Updated April 13, 2017. https://www.ncbi.nlm.nih.gov/books/NBK83985/ 7. Haffner D, Emma F, Eastwood DM, et al. Clinical practice recommendations for the diagnosis and management of X-linked hypophosphataemia. Nat Rev Nephrol. 2019;15(7):435-455. doi:10.1038/s41581-019-0152-5 8. Lo SH, Lachmann R, Williams A, Piglowska N, Lloyd AJ. Exploring the burden of X-linked hypophosphatemia: a European multi-country qualitative study. Qual Life Res. 2020;29(7):1883-1893. doi:10.1007/s11136-020-02465-x 9. Ruppe MD, Zhang X, Imel EA, et al. Effect of four monthly doses of a human monoclonal anti-FGF23 antibody (KRN23) on quality of life in X-linked hypophosphatemia. Bone Rep. 2016;5:158-162. doi:10.1016/j.bonr.2016.05.004 10. Trombetti A, Al-Daghri N, Brandi ML, et al. Interdisciplinary management of FGF23-related phosphate wasting syndromes: a Consensus Statement on the evaluation, diagnosis and care of patients with X-linked hypophosphataemia. Nat Rev Endocrinol. 2022;18(6):366-384. doi:10.1038/s41574-022-00662-x