Patient case studies of XLH
See sample case studies of adults and children.
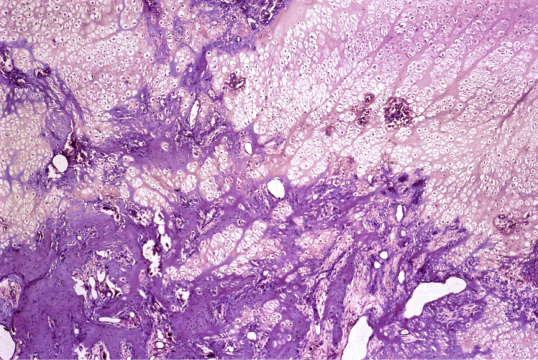
XLH can be misdiagnosed as nutritional rickets, osteomalacia, hypophosphatasia, Pyle disease, or physiologic bowing. Clinical/radiographic findings, family history, and biochemical tests can help establish a diagnosis of XLH. XLH can be confirmed through genetic testing for variants of the PHEX gene, and checking for elevated levels of FGF23 can help to further establish a diagnosis.2-4
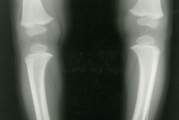
Predominant clinical findings in children include2,5-7:
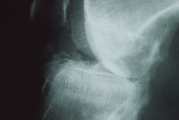
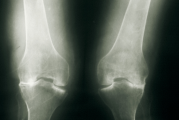
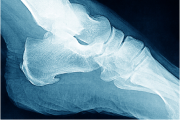
Evaluate skeletal symptoms through radiography.
Other signs and symptoms may also include8:

Adults with XLH may present with8-10:
Other signs and symptoms may also include8,11:
XLH is inherited in an X-linked dominant pattern, so a positive family history of the disease supports the diagnosis. In a family with a history of XLH, screen other first-generation family members for XLH. This can help identify previously undiagnosed individuals.12
Since approximately 20% to 30% of XLH cases are spontaneous, it’s important to ask your patient if they have a medical history of short stature, rickets, osteomalacia, osteoarthritis, and dental abscesses, all of which may indicate XLH.13
Evaluate age-normalized levels of fasting serum phosphorus for an accurate diagnosis. Low phosphorus levels and a low TmP/GFR ratio are the most relevant biochemical findings for XLH.2,12,13
| Biochemical Test | XLH |
| Fasting serum phosphorus |
 Down Down
|
| 1,25(OH)2D |
 Down or inappropriately
normal Down or inappropriately
normal
|
| 25(OH)D | Normal |
| TmP/GFR |
 Down Down
|
| ALP |
 Up Up
|
| Serum calcium | Normal |
| Urinary calcium |
Normal to decreased
|
| PTH | Normal to slightly up |
| Through a genetic analysis of the PHEX gene | By checking for elevated intact FGF23 levels in untreated patients |
| Learn more about sponsored genetic testing | Request a sponsored FGF23 testing kit* |

Prioritize testing your patient’s fasting serum phosphorus levels in addition to clinical/radiographic, family history, biochemical, and genetic findings in order to help diagnose XLH.2,12

See sample case studies of adults and children.

Watch videos to get more information about how XLH affects the body.

From case studies to brochures, find resources for you and your patients to understand more about this rare condition.
Set up time with a representative to talk more about XLH, or sign up for news and information about XLH.
References:
1. Hamilton AA, Faitos S, Jones G, Kinsley A, Gupta RN, Lewiecki EM. Whole body, whole life, whole family: patients' perspectives on X-linked hypophosphatemia. J Endocr Soc. 2022;6(8):bvac086. doi:10.1210/jendso/bvac086 2. Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL. A clinician's guide to X-linked hypophosphatemia. J Bone Miner Res. 2011;26(7):1381-1388. doi:10.1002/jbmr.340 3. Rush ET, Johnson B, Aradhya S, et al. Molecular diagnoses of X-linked and other genetic hypophosphatemias: results from a sponsored genetic testing program. J Bone Miner Res. 2022;37(2):202-214. doi:10.1002/jbmr.4454 4. Haffner D, Emma F, Eastwood DM, et al. Clinical practice recommendations for the diagnosis and management of X-linked hypophosphataemia. Nat Rev Nephrol. 2019;15(7):435-455. doi:10.1038/s41581-019-0152-5 5. Carpenter TO. Primary disorders of phosphate metabolism. Endotext. Accessed February 3, 2023. https://www.ncbi.nlm.nih.gov/books/NBK279172/ 6. Linglart A, Dvorak-Ewell M, Marshall A, San Martin J, Skrinar A. Impaired mobility and pain significantly impact the quality of life of children with X-linked hypophosphatemia. Bone Abstracts. 2015;4(P198). doi:10.1530/boneabs.4.P198 7. Skrinar A, Dvorak-Ewell M, Evins A, et al. The lifelong impact of X-linked hypophosphatemia: results from a burden of disease survey. J Endocr Soc. 2019;3(7):1321-1334. doi:10.1210/js.2018-00365 8. Linglart A, Biosse-Duplan M, Briot K, et al. Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr Connect. 2014;3(1):R13-R30. doi:10.1530/EC-13-0103 9. Trombetti A, Al-Daghri N, Brandi ML, et al. Interdisciplinary management of FGF23-related phosphate wasting syndromes: a Consensus Statement on the evaluation, diagnosis and care of patients with X-linked hypophosphataemia. Nat Rev Endocrinol. 2022;18(6):366-384. doi:10.1038/s41574-022-00662-x 10. Giannini S, Bianchi ML, Rendina D, Massoletti P, Lazzerini D, Brandi ML. Burden of disease and clinical targets in adult patients with X-linked hypophosphatemia. A comprehensive review. Osteoporos Int. 2021;32(10):1937-1949. doi:10.1007/s00198-021-05997-1 11. Mindler GT, Kranzl A, Stauffer A, et al. Lower limb deformity and gait deviations among adolescents and adults with X-linked hypophosphatemia. Front Endocrinol (Lausanne). 2021;12:754084. doi:10.3389/fendo.2021.754084 12. Ruppe MD. X-linked hypophosphatemia. In: Adam MP, Everman DB, Mirzaa GM, et al., eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; February 9, 2012. Updated April 13, 2017. https://www.ncbi.nlm.nih.gov/books/NBK83985/ 13. Dahir K, Roberts MS, Krolczyk S, Simmons JH. X-linked hypophosphatemia: a new era in management. J Endocr Soc. 2020;4(12):bvaa151. doi:10.1210/jendso/bvaa151 14. Santos F, Fuente R, Mejia N, Mantecon L, Gil-Peña H, Ordoñez FA. Hypophosphatemia and growth. Pediatr Nephrol. 2013;28(4):595-603. doi:10.1007/s00467-012-2364-9 15. Florenzano P, Cipriani C, Roszko KL, et al. Approach to patients with hypophosphataemia. 2020;8(2):163-174. Lancet Diabetes Endocrinol doi:10.1016/S2213-8587(19)30426-7